Cataract
Basics
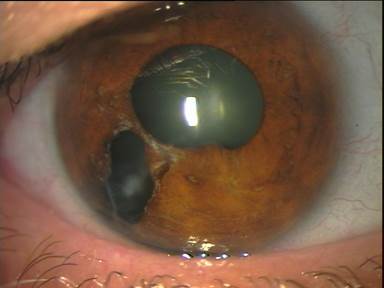
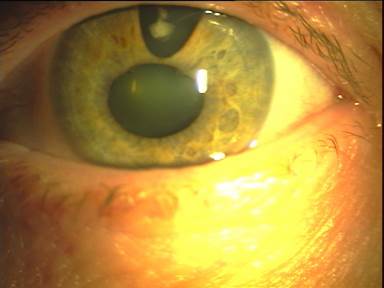
The cataract denotes a turbidity of the eye lens. In a case of an advanced cataract one can recognize the gray or whitish turbidity behind the pupil. This is how the name came into being in German-speaking countries. Cataract (or cataracta) means waterfall or "falling down", which was inspired by the waterfalls in the upper Nile. More about the cataract can be found on Wikipedia.
Almost every second person over the age of 65 is more or less affected by cloudiness of the eye lens. The treatment alternatives are based on the replacement of the opaque eye lens with an artificial lens. A drug therapy is not possible so far. Cataract surgery is the most commonly performed surgery on humans worldwide. In Germany over 600,000 eyes are operated annually.
Diagnostics
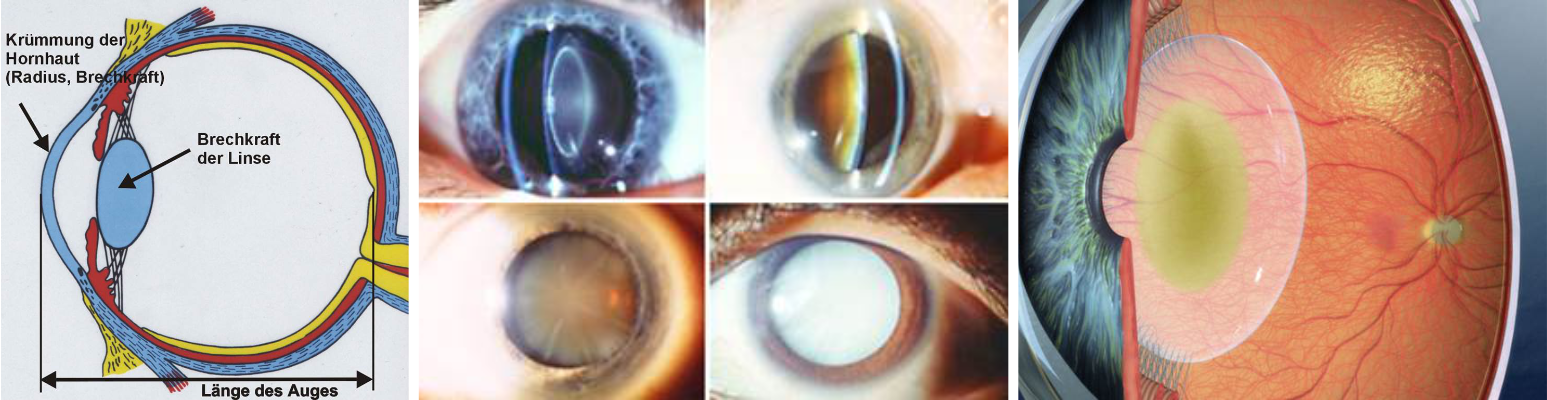
Before surgery, of course, the eye must be thoroughly examined organically. In addition, the eye is measured in order to calculate the refractive power of the lens, that is to be used. These include measurement of the corneal radii, the total refractive power of the eye, examination of visual acuity, axial length measurement, etc.
To optimize the overall result, further investigations are possible and useful.
Example from our current standard:
For the LASICAT treatment further investigations are added to allow a personalized reduction of corneal astigmatism (see also Cataract surgery / LASICAT).
Cataract surgery

Overview
Together with the patient, we select the best possible procedures. In the operation of the "cataract", the clouded lens is exchanged with an artificial lens (intraocular lens = IOL). The goal for the patient such as the surgeon is usually a result without residual refraction, meaning glasses will not be necessary. The strategies and options vary depending on the type of intervention.
Prerequisite is a thorough diagnosis, examination and measurement (see "Diagnostics")
The cataract surgery as the refractive lens exchange is usually composed of the following sub-steps:
- Applying the cuts to the eye (for later insertion of the instruments and implantation of the IOL)
- Opening the lens ("Capsulorhexis")
- Shredding of the lens contents by laser or ultrasound ("Phacoemulsification") and suction of the tissue (only the capsule remains)
- Implantation of the artificial lens
In the previous standard method ("phaco", ultrasound comminution of the lens and suction) all steps are performed manually by the surgeon.
Current treatment methods
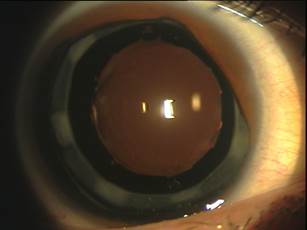
Phacoemulsification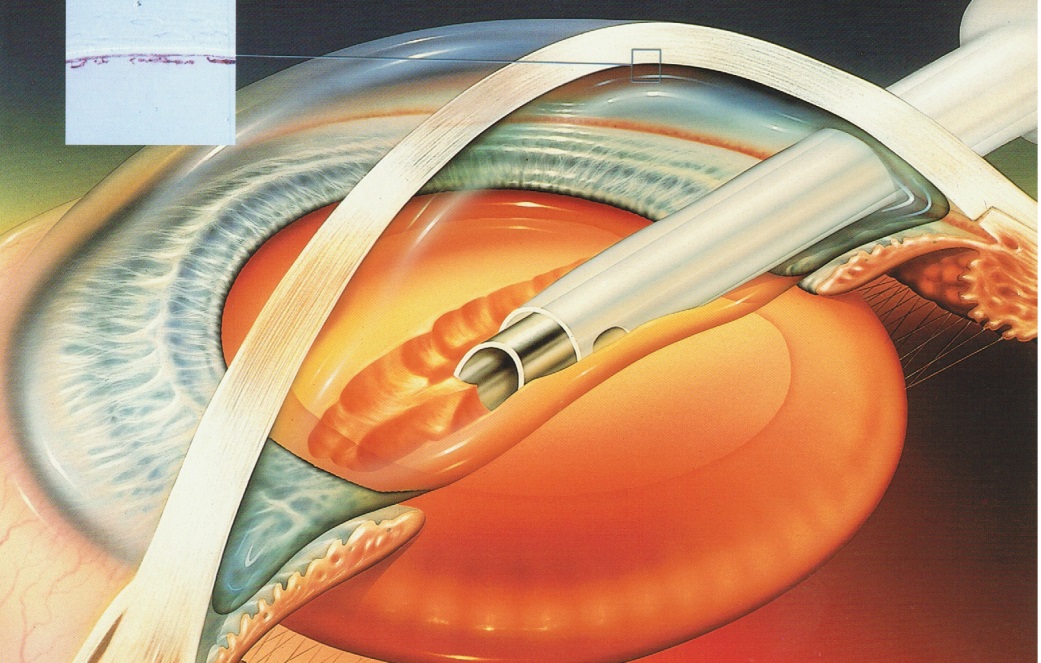 In order to be able to implant the new, clear artificial lens in the eye, the cloudy lens must first be removed from the eye. For this purpose instruments are inserted into the eye via small incisions on the edge of the cornea, only then opening the anterior capsule of the lens as circularly as possible. By means of ultrasound energy, the lentil core is comminuted or "emulsified" via a small tube and aspirated with the lens cortex. The capsule should be preserved during this process, because then the artificial lens is to be implanted into the capsular bag.
In order to be able to implant the new, clear artificial lens in the eye, the cloudy lens must first be removed from the eye. For this purpose instruments are inserted into the eye via small incisions on the edge of the cornea, only then opening the anterior capsule of the lens as circularly as possible. By means of ultrasound energy, the lentil core is comminuted or "emulsified" via a small tube and aspirated with the lens cortex. The capsule should be preserved during this process, because then the artificial lens is to be implanted into the capsular bag.
CataPulse
Since the use of ultrasound in particular can damage the cornea, work has been going on for years on alternative methods for phacoemulsification. In the CataPulse process, the lens contents are removed by a high-frequency pulsed vacuum.
LASICAT
LASICAT - Femtolaser assisted cataract surgery
History
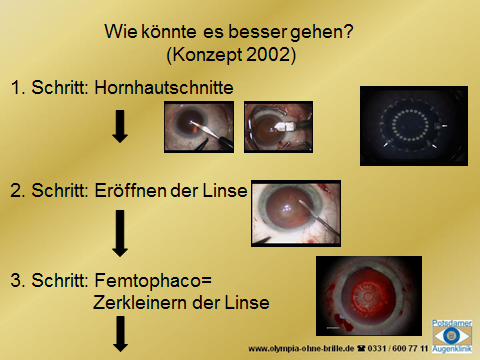 Based on the possibilities offered by the femtosecond laser, in which the "Femto-Lasik" performs a high-precision surface incision in the cornea, we conceived a derivative approach for cataract surgery: incisions into the cornea to introduce the instruments and implantation of the IOL and astigmatism correction, for the precise opening of the lens and for shredding the contents. Based on the possibilities offered by the femtosecond laser, in which the "Femto-Lasik" performs a high-precision surface incision in the cornea, we conceived a derivative approach for cataract surgery: incisions into the cornea to introduce the instruments and implantation of the IOL and astigmatism correction, for the precise opening of the lens and for shredding the contents. |
Initially, the concept was of no interest to the industry, because the time was not yet ripe. Also patent application (2003) and lectures and congress films (2004) were virtually ignored. We named the concept "LASICAT Lasers in Cataract Surgery" in 2004 at the ASCRS in San Diego, the Allergan Symposium in Arizona, DOC in Nuremberg and ESCRS in Paris.
 In 2010 it was time. Four companies showed their development at the World Congress in Berlin. In the following years, we observed the individual device solutions. In 2014, we decided on the concept of LensAR and introduced the first system in Berlin and Brandenburg into our practice. In 2010 it was time. Four companies showed their development at the World Congress in Berlin. In the following years, we observed the individual device solutions. In 2014, we decided on the concept of LensAR and introduced the first system in Berlin and Brandenburg into our practice. |
Procedure od the operation with the LensAR-Laser
Before the laser treatment, a contact lens is placed on the eye of the patient. This so-called patient interface will be followed by a last online diagnosis. The laser is centered over the lens of the eye and the eye is measured via a 3D camera system. Thereafter, the treatment planning takes place. Within seconds, the system creates a treatment proposal that is controlled by the surgeon and modified if necessary. The actual laser treatment steps follow one after the other:
- The circular opening of the anterior lens capsule (capsulotomy)
- The crushing of the natural lens
- The incisions in the cornea
- Possibly additional intra-corneal incisions to correct astigmatism
Which steps does the surgeon perform manually?
The surgeon plans and monitors the entire procedure with the help of the camera system of the laser. After the comminution of the natural lens by the laser, the patient is oberserved with a surgical microscope in a second treatment step, while the surgeon carefully sucks the interior of the crushed lens with a special instrument and possibly with ultrasound support, similar to the previous standard. LASICAT surgery requires significantly less ultrasound energy than without a laser. This is always dependent on the hardness of the natural eye lens. Finally, the surgeon implants the previously folded artificial lens into the now empty capsular bag and centers it.
Why is the lens operation with the laser more precise?
We have been working on the treatment of defective vision with the femtosecond laser for many years, including the so-called femto-Lasik (in more than 90% of our cases). An incision with the femtosecond laser can be made at any depth without surgically opening the eye. Because the operation is performed on the intact eye, the sections of the femtosecond laser are independent of external factors and therefore reproducible. They are sturdier and more accurate than manually guided cuts and their design is precisely plannable. For this reason, the opening of the lens capsule generated by the laser is circular with clear edges, while the cut architecture deviates from manual incision and also depends on the experience of the surgeon.
Why can the laser achieve a better visual outcome?
An optimal visual result requires an exact positioning of the lens. Small deviations can have a negative effect. Precise planning of the laser incisions allows for more precise placement of the lens, resulting in a higher percentage of better vision than traditional manual lens surgery.
Why is laser surgery more gentle?
Among other things, the LensAR laser grinds up the natural lens, making it easier to remove the lens nucleus. In order to aspirate the particles, the surgeon now requires significantly less ultrasound energy than without the use of lasers. This protects the tissue structures of the eye, especially the endothelium of the corneal surface. In addition, during the procedure, other structures in the eye are less stressed.
Why is laser surgery safer?
Since the LensAR laser can cut much more precisely than any experienced surgeon, the application is considered safer overall. Nevertheless, the surgeon should also have a lot of experience in the use of lasers in order to be able to carry out all operation steps exactly. The experiences from operations with different femto-cataract lasers show significantly fewer complications.
How will development continue?
Since autumn 2015, we now have the further development of the LensAR available. With the personalized "Streamline treatment", it is now possible to automatically work with more laser energy with harder lens cores, or with softer ones with correspondingly less laser energy. That makes the process even more gentle. Similarly, we can now make corrections of astigmatism semiautomatic. For this purpose, the measurement result of a special corneal topography is transmitted directly to the laser and arcuate incisions are placed in the cornea.
Advantages of LASICAT in the Potsdam Eye Clinic in the Graefe House (Overview):
- Incisions in the cornea are computer-aided and thus more precise
- Correction of existing astigmatism
- High-precision computer-controlled opening of the lens capsule
- simplified removal of the body's clouded lens
- less phaco (ultrasound-) -energy protects the corneal endothelium
- less tension on the zonular fibers of the lens
- less pressure fluctuations during the operation, higher stability of the eye
- Online diagnostics and monitoring of treatment via 3D camera, computer controlled
- Accurate placement of the IOL as the basis for better vision
- if necessary, fine laser correction possible in the clinic (LASIK or PRK)
- if necessary, combination with PTK possible
Own contributions:
For the development of surgical techniques in cataract and lens surgery, we have already been able to make some innovative contributions to the use of laser technology:
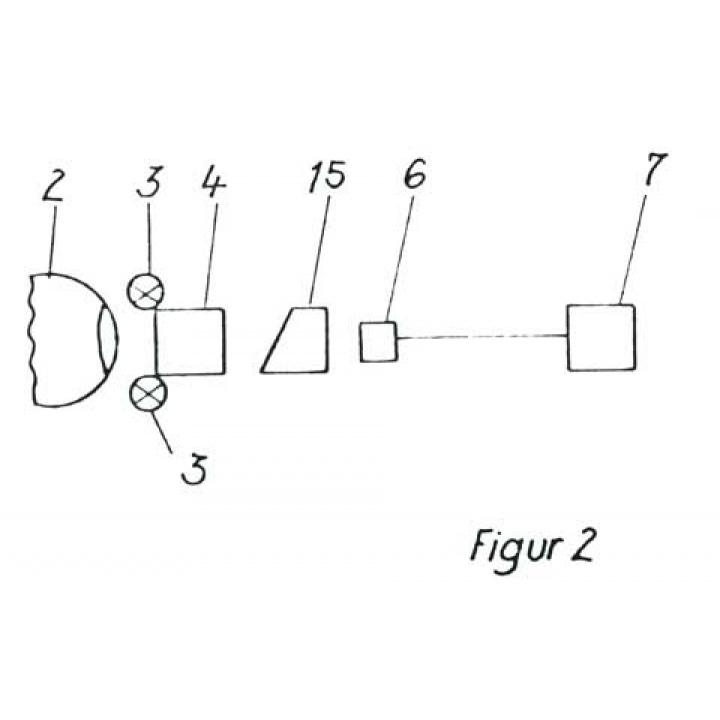
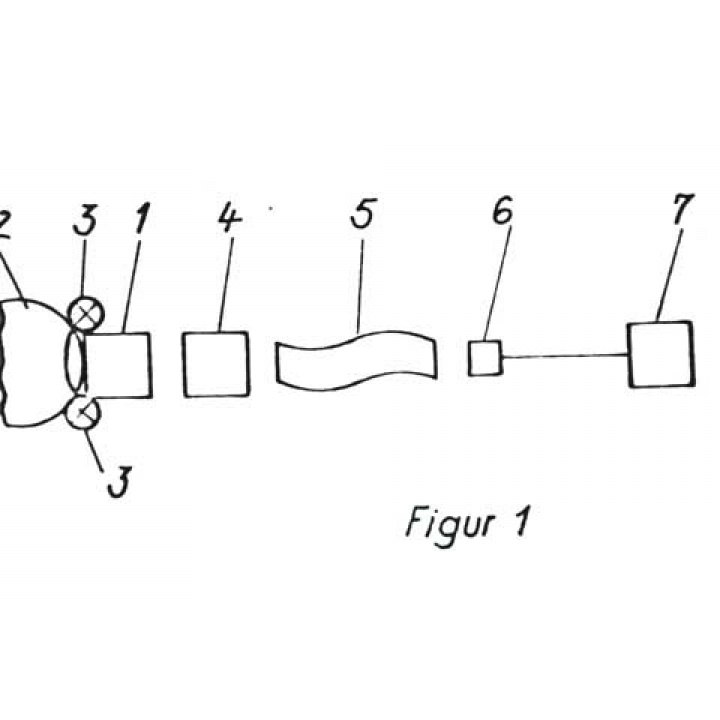
- As early as 1985, the concept of the so-called "laser phaco". The lens is directly comminuted and aspirated via a probe introduced into the eye (patent application 1985 and 1997).
- When using the femtosecond laser corneal cuts and opening and crushing of the eye lens are made via contact optics. Our concept of femtolaser application was developed in the years 2002-2003. Patent applications were filed by us in 2003, 2009, 2013 and 2014.
Congressional contributions:
- Rasch, V .: "LASICAT-Lasers in Cataract Surgery", video contribution to the film festival of the ASCRS, San Diego 2004
- Rasch, V .: "LASICAT Laser in Cataract Surgery", video contribution at the DOC, Nuremberg 2004
- Rasch, V .: "LASICAT Lasers in Cataract Surgery", First Experience with the LaserSoft, Lecture ESCRS, Paris 2004
- Rasch, V., Majewski, S .: Limiting aspects in LASICAT surgery (Femto Phaco), poster presentation WOC (World Congress) Abu Dhabi 2012
Of the many terms used today for the same procedure of femtolaser-assisted cataract surgery, we use our 2004 propagated term "LASICAT Lasers in Cataract Surgery".
Nomination: Femto-Phaco + LASICAT were nominated for the "Brandenburger Zukunftspreis CAI 2013" in the category "Innovation".
Femto-Phaco + LASICAT were nominated for the "Brandenburger Zukunftspreis CAI 2013" in the category "Innovation".
Implantation
As soon as the lens contents are crushed and aspirated, the remaining capsule cleaned and a so-called viscoelastic filled in the capsular bag and the anterior chamber, now follows the implantation of the artificial lens. In today's usually used folding lenses, the IOL is folded in a cartridge and implanted depending on the type of lens over an incision of 2-2.8 mm and centered in the capsule. Finally, the viscoelastic is sucked off again.
IOL-principles
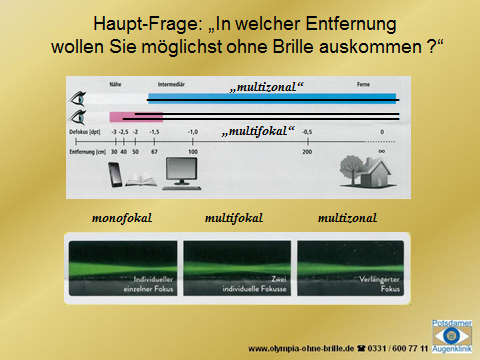
In addition to the standard monofocal IOL, various special lenses have been developed that have special optical features for specific purposes:
- Multifocal and multizonal IOLs (for viewing at different distances)
- Toric IOL (to correct higher astigmatism)
- LAL (Light Adjustable Lens) with the ability to post-correct implanted lenses in the eye regarding the refractive power
- Macula lenses
- Filter lenses: All modern lenses have UV protection today. Undertow. Blue light filter lenses (often appear yellow) also have protection against "blue light".
- Optical irises: Especially for defects of the iris or albinism
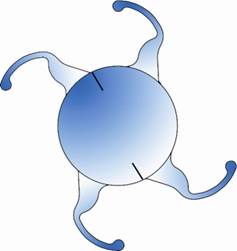
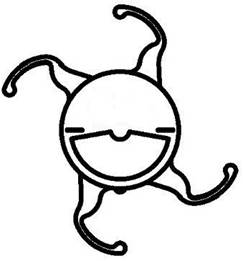
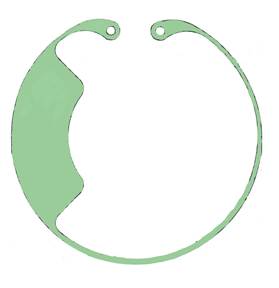
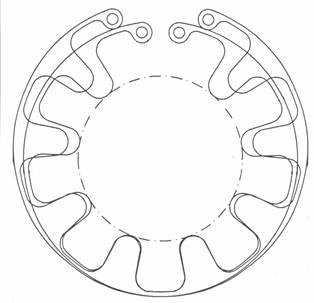
All IOLs consist of an optical part responsible for the way of seeing. The so-called haptic realizes the fixation in the eye. In the development of the intraocular lenses, there were a variety of design variants. The support in the capsular bag was formerly mostly at 2 points or zones. In 1994 we designed a support with 4 zones, which is modified many times until today:
- with closed haptics
- or with our favored open haptics, the so-called "turtle design" (see cataract / research)
Monofocal IOL
The optics of the lens can be compared to a lens with a focal point, so for a look into the distance or for reading (spherical IOL). A special form is aspherical IOL. These take into account the uneven refractive power of the cornea from the center to the periphery, allowing a sharper vision. They are among the "premium lenses".
Multifocal lenses (MF-IOL, MIOL)
 With standard intraocular lenses, only in the ideal case an independence of glasses for the distance can be achieved. Vicinity will always require reading glasses. On the other hand, so-called multifocal intraocular lenses of different construction give the patient the possibility of freedom from glasses both for the distance and for the vicinity. With standard intraocular lenses, only in the ideal case an independence of glasses for the distance can be achieved. Vicinity will always require reading glasses. On the other hand, so-called multifocal intraocular lenses of different construction give the patient the possibility of freedom from glasses both for the distance and for the vicinity. |
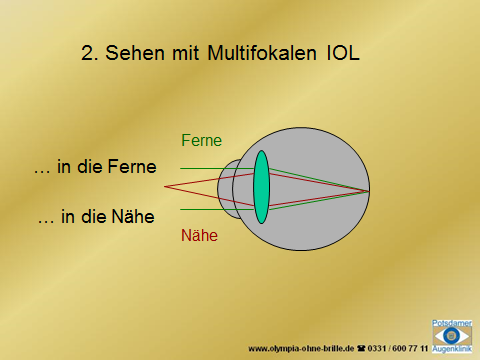 Multifocal lenses come closest to seeing naturally, as with a healthy eye. At work, in sports or in the hobby, wherever the patient relies on good vision in the distance and in the vicinity, these lenses offer a good solution, because glasses can usually be dispensed with. However, certain trade-offs in terms of optical quality and visual acuity still need to be made. Multifocal lenses come closest to seeing naturally, as with a healthy eye. At work, in sports or in the hobby, wherever the patient relies on good vision in the distance and in the vicinity, these lenses offer a good solution, because glasses can usually be dispensed with. However, certain trade-offs in terms of optical quality and visual acuity still need to be made. |
Goal of the operation with multifocal lenses
|
With such multifocal lenses, which have flat zones for distance and near, the far-near effect may be absent with a very narrow pupil (for example, in very bright sunlight). For medium-wide pupils (normal case), a vision in the distance and in the mid-range without glasses should be possible. If the pupil is wide, there may be "halos" or other appearances around lights or objects (e.g., in the dark). However, most patients tolerate this after a few months. For example, professional drivers should therefore refrain from a multifocal lens. Eventually, the contrast vision is lowered. For reading with multifocal lenses of very small writing, reading glasses are still required. This is possible due to different optical principles. |
How certain is it, that the patient with a multifocal no longer needs glasses after surgery? In the case of astigmatism, there is no focal point in the eye, but so-called focal lines in mutually perpendicular axes. The youthful, healthy eye or monofocal IOL eye can tolerate this to some extent. This is more difficult with multifocal IOLs. If there is an astigmatism of 0.75 dioptres after surgery, there may be visual disturbances, which can be corrected if necessary. But this is individually very different. Sometimes astigmatism also produces shadow vision, e.g. on letters. LASICAT II can already reduce astigmatism during surgery.
In the case of astigmatism, there is no focal point in the eye, but so-called focal lines in mutually perpendicular axes. The youthful, healthy eye or monofocal IOL eye can tolerate this to some extent. This is more difficult with multifocal IOLs. If there is an astigmatism of 0.75 dioptres after surgery, there may be visual disturbances, which can be corrected if necessary. But this is individually very different. Sometimes astigmatism also produces shadow vision, e.g. on letters. LASICAT II can already reduce astigmatism during surgery.
A remaining "residual refraction", meaning the spectacle value for the distance, can be reduced by laser treatment of the cornea. This also applies to astigmatism. The additional costs depend on the selected laser process.
Even with mutifocal IOL, visual acuity of 100% (or better) can be achieved without glasses. However, the focal points in the different target ranges are not as sharp as in a healthy eye. Thus, the image on the retina may be a little blurred. This is also noticeable in the intermediate distances.
Other possible restrictions
Since the light is divided from far and near, less light comes into the eye from every distance. This makes the picture seen a bit darker. The contrast vision is reduced. You may need a bit more lighting (for example, when reading) than with a simple, monofocal IOL or earlier in adolescence. Grayscale in certain texts may be worse recognized. Even when driving at dusk, a contrast reduction can interfere.
With multifocal IOLs, stray light or glare sensations can also occur at the edges or transitions. This can lead to light halos, being seen around lights at night. People who drive a lot at night should therefore not receive MF IOL.
There is also a picture size change by the operation at higher glasses strengths. This is particularly noticeable when replacing a clear lens (CLE), as th expectation of this is higher than in a case of advanced cataract. - In case of hyperopia postoperatively: image reduction, - In case of myopia postoperatively: image magnification. For both refractive errors, the higher the diopters, the greater the effect. Also: when correcting high hyperopia, there may already be a visual acuity reduction due to the smaller image. (The effect was demonstrated.)
The IOLs are usually used in the natural, freed from the lens opacification capsule. If these break during the operation, it may not be possible to implant the planned multifocal IOL. Another model could be useful later.
Occasionally, present or later emerging capsule opacities ("capsule fibrosis") can affect vision on multifocal lenses more than standard IOL. For this reason, it should be checked in the first few months whether a visual gap using the YAG laser makes sense. This treatment is done sitting down, by the way it is covered by insurance.
Both the evaluation of the healing process and the verification of the accuracy of the measurement and implant, and thus also of the quality assurance, must be attended by the patient. With unforeseen complications on the first eye, the planning for the second eye changes. After one-sided operation, there may also be a side difference in brightness and color vision. In rare cases, an explant may even be desired with the exchange for a monofocal IOL.
We need to know that, as in other areas, there are measurement inaccuracies or tolerances. This - on the one hand - concerns the lens operation the diagnosis (despite multiple measurements on different devices), the accuracy of the implants (these are usually graded in 0.5 dioptres), but also the later position of the intraocular lens in the eye. Most of the time, we are aiming for a +/- 0 diopters refraction for the leading eye. The other eye may possibly be planned a bit in minus (monvision or micro-monovision).
Despite all measurements and calculations before the operation, there may be deviations from the target refraction. This is mainly dependent on the distance between the inserted new lens and the cornea (so-called anterior chamber depth). The anterior chamber is lower after surgery than before surgery. The anterior chamber depth can not be accurately estimated or calculated. As a result, in individual cases after surgery, additional correction by glasses may be required for the distance. This is a possible and unpredictable, individual problem of the eye of a patient, which can occur with all intraocular lenses and is not the responsibility of the surgeon.
In the healing process, the opening size and shape of the so-called Kapsulorhexis can play a role. Therefore, we recommend the use of the femtosecond laser (LASICAT) for an exact rhexis, but of course also as a more gentle surgical procedure for all lens operations. Multifocal, multizonal and toric intraocular lenses are only implanted in conjunction with LASICAT.
Contraindications when deciding on multifocal intraocular lenses
Multifocal IOLs are manufactured with high precision. Optical errors in the IOL optics would be more noticeable with these lenses than with standard IOLs. The same applies to limitations in the optics of the eye. Therefore, we implant e.g. no multifocal IOL in a case of...
- ... corneal scars or
- ... changes in the corneal endothelium (cornea guttata)
Likewise, there should be no macular changes. Even driving at night is often problematic with multifocal IOL.
"Multizonal" intraocular lenses
In this group of implants, we include those IOLs that do not have a unique far and near point, such as multifocal (bifocal or trifocal) lenses. However, in contrast to monofocal IOLs, they make it possible to see from far away to a "middle" close range, i.e. "multizonal". They show good visual acuity, but are mostly inferior to the multifocal lenses at a reading distance of 30-40 cm. There are also different optical principles here. The visual "side effects" and concomitants as with multifocal IOL are usually lower in multizonal IOLs.
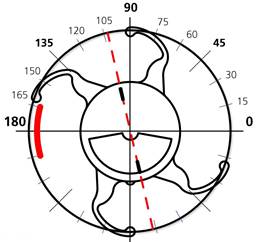
Toric IOL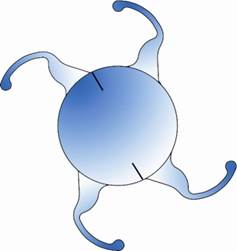  If, in addition to the opacity of the eye lens, there is greater astigmatism, Toric lenses are used. They reduce the total astigmatism of the eye and thus the most congenital distorted vision. Together with the industry, we developed the first "personalized" Toric IOL worldwide. In August 2005 the implantation of these lenses was started in our clinic. If, in addition to the opacity of the eye lens, there is greater astigmatism, Toric lenses are used. They reduce the total astigmatism of the eye and thus the most congenital distorted vision. Together with the industry, we developed the first "personalized" Toric IOL worldwide. In August 2005 the implantation of these lenses was started in our clinic. |
LAL - Light Adjustable Lens
Why?
The goal of cataract surgery is usually a vision without glasses after surgery, thus the achievement of a residual gland value below +/- 0.5 dioptres. In spite of extensive preoperative diagnostics, improved surgical techniques and precision in the IOL production, especially in the postoperative anterior chamber depth, the causes are the distance of the inserted new lens from the cornea. This can not be reliably predicted despite a thousand-fold observations in individual cases.
A revolutionary further development now solves this problem: the Calhoun Light Adjustable Lens can be "fine-tuned" by precisely metered UV irradiation even after implantation. This principle of postoperative correction of an intraocular lens was developed by Prof. Robert Grubbs, one of the Nobel Laureate for Chemistry 2005!
We have been implanting this IOL since June 2008. Since 2011, we have been implanting this IOL in conjunction with additional protective shields in the eye to reduce stray light during UV irradiation. For this we have filed a patent application.
Macula lenses
The eyemax mono is an artificial lens designed specifically for patients with macular disease. The most common cause of macular damage is age-related macular degeneration (AMD). This leads to distortions or to the failure of the central vision and thus the ability to read and to recognize faces.
The eyemax mono supports the ability of the brain to use the most functional areas of the macula for a sharp image. The image seen is not only projected on the macula center(as usual), but also on border areas.
Due to the complex optical surface production, the eyemax mono is located in the high-end premium segment.
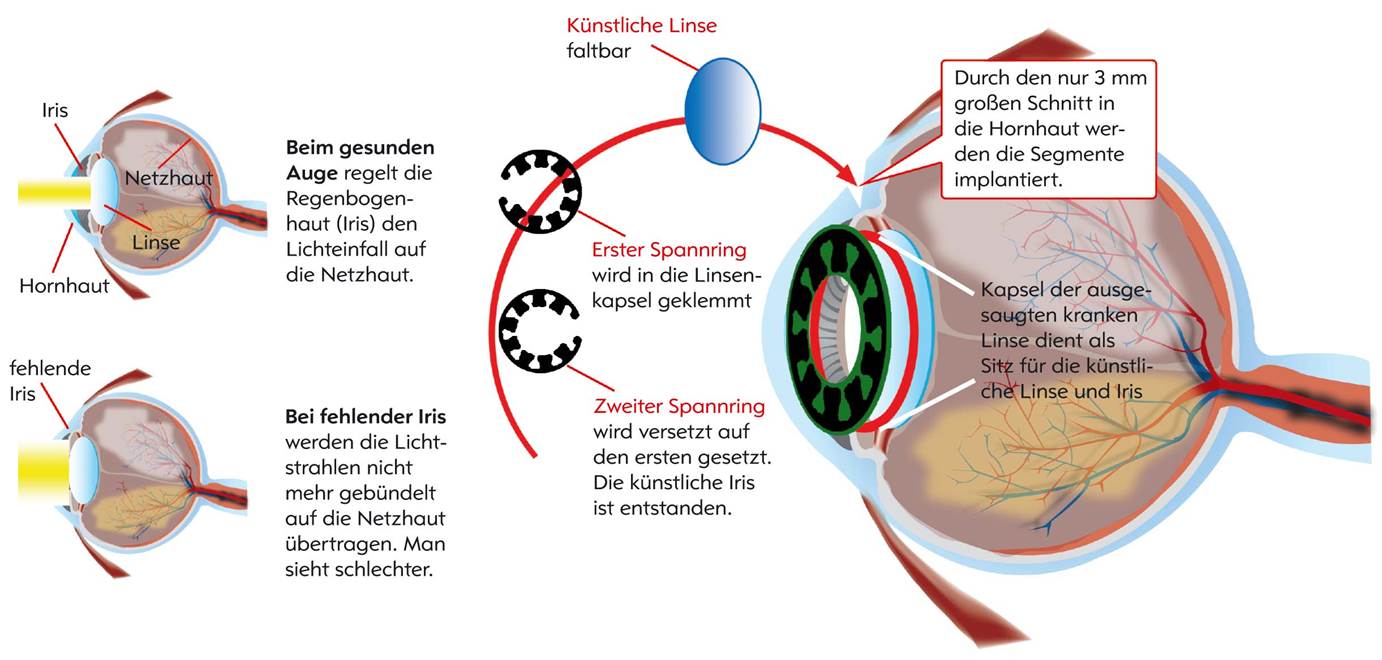
Special implants
In addition to the intraocular lenses (for optical correction), there are various implants with special tasks, e.g.
- Capsular tension rings
- Capsule tension rings with Coloboma aperture
- Capsular tension rings with iris aperture
- ring apertures
- and others
Find out more about the special implants we developed under "Cataract / Research".
Research
- Instruments and methods
- Implants - IOL
- Capsular tension rings
- Ring aperture
- Basic research and concepts
Instruments and methods
For nearly 40 years, we have been involved in major developments in cataract and lens surgery. Since 2008 we cooperate with VR Vision Research GmbH in our house in many development topics.
Here are some examples from the past:
Removal of the eye lens
- Crushing of the eye lens by means of optical energy, "laser phaco", with a patent application 1985
- 2002 concept "Femtokatarakt", with a patent application 2003
- 2004 Presentation of the concept (LASICAT, Video ASCRS 2004 in San Diego) > Video
- "Limiting aspects in LASICAT", Poster WOC AbuDhabi 2012
Surgical instrumentation / procedure
- Cannula for capsular polishing, Pat. Application 1989
- Ultrasonic polishing of the lens capsule, registration 1999
- Holding tweezers for ICL cartridges (Cartridge Holder, Katana, USA)
- Implantation spatula tweezers (Deutschmann, Zittau)
- Head positioning system for eye surgery, Pat. 1988
- Irrigation hook with iris retractor, "Irrigation hook" (Geuder, Heidelberg)
- Installationskanüle für Vision Blue bei Cat. mat. (Fa. Bausch& Lomb, D)

- TCI Topography Controlled Incision, 2002
- "TDI - a new concept in refractive cataract surgery", Array-roundtable, AMO, Kiel, 5.7.2003
- TDI - Topography double incision, Poster, Lecture
- WORCS (Wavefront Oriented Refractive Surgery), 2001, 2002
- "Managing Astigmatism in Cataract Surgery: MICS, TDI, toric IOL or LASICAT?", Afro-Asian Congress of Ophthalmology, Istanbul, 18.-22.6.2004



Implants - IOL
From 1984 to 1990 work was done on building up an IOL production for GDR needs. Shortly before completion of the project, it was canceled due to the new economic situation.

Development of a new IOL design: the "Turtle-IOL", patent applications 1996, 2000 (for the correction of individual aberration), 2006.
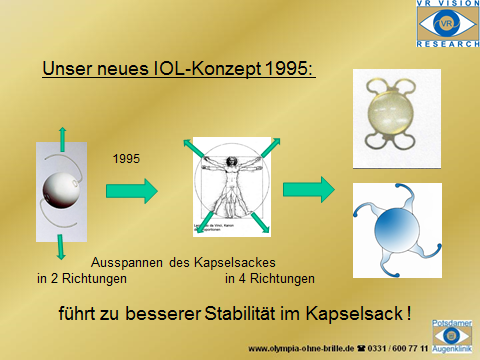
This resulted in different design variants (selection):
The Oculetnis IOLs are offered in different versions.
Capsular tension rings
Capsular tension rings serve to relax the lens capsule. They are inserted into the (endogenous) lens capsule during lens surgery.
- Patent Application "Capsular Tension Ring", 1996
- "New Type of Capsular Tension Rings", post-competition, ASCRS San Diego 1998 (prize for best poster)
- "A New Type of Capsular Clamping Rings", Poster, DOC Nuremberg 1999 (Posterprice)
- "CTR with Coloboma and Iris Aperture: An Alternative to Patients with Large Iris Defects Aniridia or Albinism".
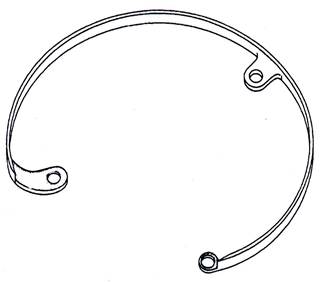

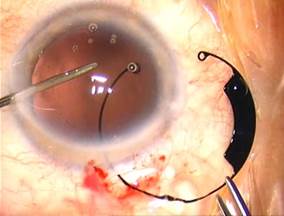
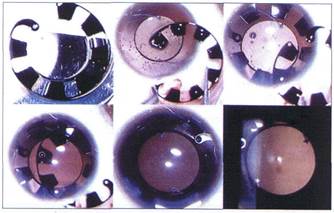
Capsular tension rings with Coloboma aperture
The research successfully carried out in our company and in cooperation with other companies and clinics has already led to numerous patent applications and publications, for which we have, among other things, received international awards and recognition. For example, together with Morcher (Stuttgart), we are developing new implants for patients with iris defects.
In addition, we received the coveted "Oscars" for three consecutive years with our surgical films presented at the American Society of Cataract and Refractive Surgery congresses on capsule collars with iris and colo-iris diaphragms:
- 1997 K. J. Rosenthal, USA, V. Rasch, "Capsular Tension Rings with Iris Diaphragm or Colobom Aperture",ASCRS, 1997 San Diego
- 1998 V. Rasch, "Insertion of Iris Diaphragm Ring, Small Incision Cataract Surgery, and "Sutureless" Phacotrabeculectomy in a Patient with the Axenfeld-Rieger Syndrome: First Reported Case". Videocompetition of ASCRS, Boston 1998(runner up)
- 1999 B. Osher, USA"Implantation of Capsular Tension Rings with Coloboma Aperture and Iris Diaphragma into a Patient with Albinism: First Reported Case." Videocompetition of ASCRS,San Diego 1998, (runner up)

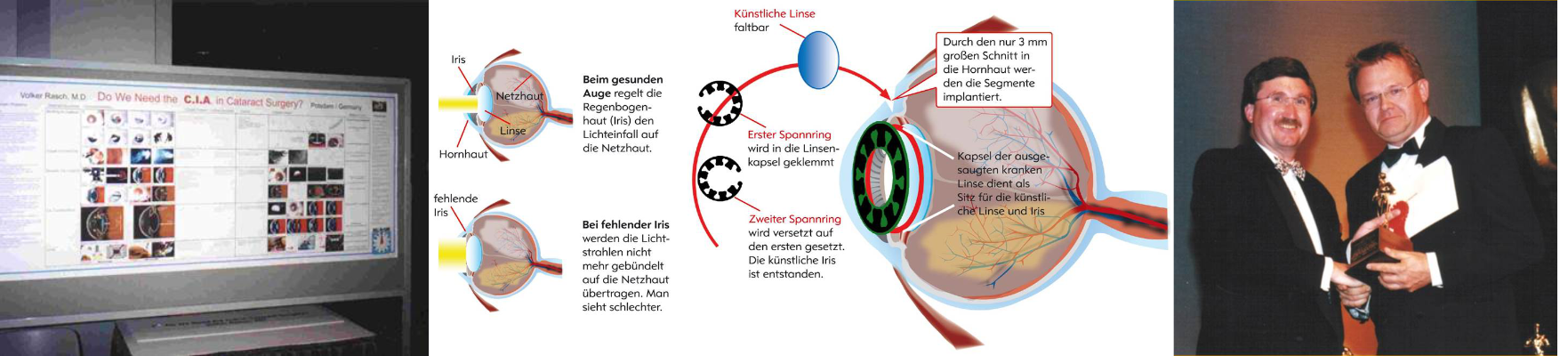
The segmented platelets cover defects in the iris. The light is thus prevented and reduces glare. They are used in partial (peripheral) iris coloboma, total iris coloboma, in albinism. Various model variants were produced.



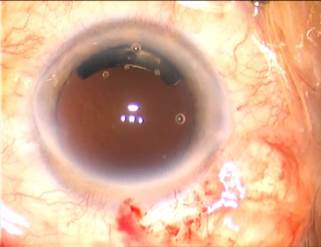
Capsular tension rings with iris aperture
With complete or almost complete absence of the iris, capsular tension rings with a plurality of segments may make sense. If two rings are implanted and slightly offset from one another, the gaps between the segments can be optically closed. These rings can also be used in albinism.
- "Artificial Iris System", patent application, 1998
- "Capsular Tension Rings with Iris Diaphragm or Colobom Aperture", K.J. Rosenthal, USA, V.Rasch, Potsdam
Further designs of implants
- Implant for the correction of aberrations, patent application 2000
- Endocapsular implant (capsular diaphragm) for toric IOL, (Fa Morcher, Type 50 A, 1996)
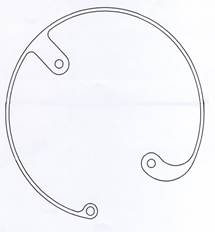
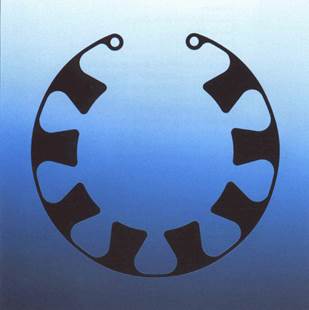
Ring aperture
For special questions, closed apertures can also be implanted in the capsular bag as an alternative to the capsular tension rings with iris apertures. In the case of UV irradiation of LAL-IOL, the retina can thus be protected against possible damage. These apertures were developed by us (VR Vision Research GmbH) together with the company Morcher / Stuttgart and implanted in the eye clinic for the first time in 2015.
For other indications (eg irreversible mydriasis, aniridia, albinism) or IOL, the inner diameter is smaller, 4mm.
Basic research and concepts
All our ideas, concepts and the resulting developments spring from the questions of everyday life. The goal is always to improve the diagnosis on the eye or the quality of our operations. With our contributions we help to improve eye surgery worldwide.
- LASICAT - femtolaser-assisted cataract surgery (see cataract> cataract surgery > LASICAT)
- "Multi-functional diagnostics"
Until the 1980s, ophthalmological diagnostic devices were each developed for a research task, designed to be almost monofunctional.
Examples would be:
- Slit lamp
- Refractometer
- Keratometer
- Ocular tonometer, and others
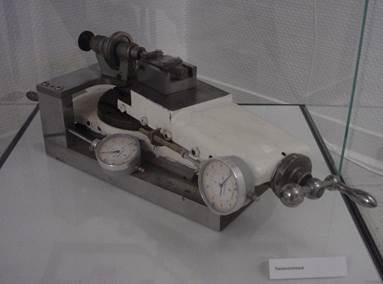
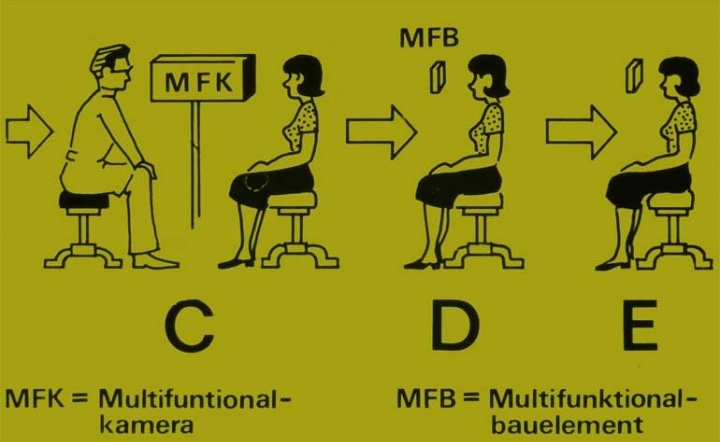
Patients had to move from device to device (Figure A). The process of improved examination units on which e.g. Slit lamp and keratometer were arranged (B). Also on the slit lights came zoom-in accessories such as Hruby lens or applanation tonometer (B). Our first concept developed in 1983 was to be able to carry out a large number of different diagnostic measurements by means of additional optoelectronic illumination systems. The image was taken by a CCD matrix camera.
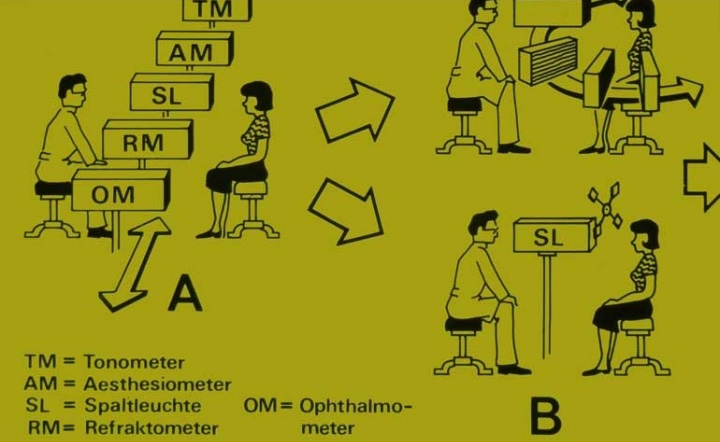
At the time, we were able to realize from the structure of the slit lamp using our own power:
- in contactless mode: electronic corneal topography
- in contact mode: Electronic applanation tonometry (see Glaucoma research)
Experimental setup and basic solutions of a multifunction camera (C) were shown at several fairs in the GDR and Hungary. A commercial realization was not possible for us at that time.
In addition to a patent application for multifunctional diagnostics (C), a "multifunctional" optoelectronic component (D) was also designed, which for the first time combined emitter and sensor on one chip. Added to this was the optoelectronic combination of diagnostics and therapy in one system (E).
- Concept for combining and integrating different diagnostic objectives in one system, "Multifunctional diagnostics"
- Patent application (DD 233299, 1984)
- Patent application 1984
The first presentation of the corneal topography by means of annularly arranged LEDs on a slit lamp took place in 1988.

- "Investigations on corneal topography with modified new projection systems", V.Rasch, Lecture Contact lens meeting Bad Hofgastein 1988
Varia:
- "Do we need the CIA in Cataract Surgery? Endoscopic follow-up during a cataract surgery: Initial Record January 13, 1999 Potsdam", published in Videocompetition of ASCRS Seattle 1999, Videocompetition of DOC Nuernberg 1999
- "Do we need the CIA in Cataract Surgery?", Videocompetition, XVI.Congress ESCRS, Vienna 1999, 2nd prize, Art.Cat.
- "Interface cleaning by I/A-Tunnel-Technique – case report
- "Topographie oriented Double-Incision (TDI) – a new concept in refractive Cataract surgery", ESCRS Munich, 06.-10.09.2003
- "Topography-Oriented Double Incision – A new concept for Managment of Astigmatism in Refractive Cataract Surgery", ASCRS, San Diego, 01.-05.05.2004
- "Laser in Cataract Surgery – LASICAT", Afro-Asian Congress of Ophthalmology, Istanbul, 18.-22.06.2004
- "Topography oriented Double-Incision (TDI) – a new concept for management astigmatism in refractive Cataract surgery", Afro-Asian Congress of Ophthalmology, Istanbul, 18.-22.06.2004
- "Topographie oriented Double-Incision (TDI) – a new concept in refractive Cataract surgery", ESCRS Paris, 18.-22.09.2004
- "Laser in Cataract Surgery - LASICAT", ESCRS Paris, 18.-22.09.2004
- "Management and implantation of the Acriflex 62 Toric IOL", ASCRS, San Francisco, 17.-22.03.2006
- "Management and Implantation of the ACRFLEX 62 VR TI - the First Personalized and Individually Produced Toric IOL First Results.", DOG, Nuremberg, May 25-28, 2006
- "Management and Implantation of LU 804 VR-T (Toric Individual) the first individual produced toric IOL." XII. Oph. Balticum, Riga, 24.-26.08.2007
- Collaboration on basic research and development of wavefront-guided diagnostics and development of new laser technology Volker Rasch, Axel Weber
- "Reproducibility and Reliability of the Wavefront Analysis by Zywave Aberrometer - Influences of Zywave, by Patients and Examiners", Posterpräsentation, 5th ESCRS Winter Refractive Surgery Meeting, Cannes 2001, prize of congress
FAQ

Is there an age limit for a cataract surgery?
Since the patient's organism is hardly affected by local anesthesia, this surgery can take place at any time.
Is a cataract surgery painful?
The local anesthetic makes the eye and its environment insensitive, so that the procedure causes no pain.
How long does cataract surgery last and how does it work?
Before surgery, pupil-dilating drops are administered. In the operating room then the local anesthesia takes place. Monitoring of blood pressure, heart rate, ECG and oxygen saturation during the entire operation is always guaranteed. The actual surgery lasts about 15-30 minutes. While doing so, the patient has to lie quietly. Subsequently, the operated eye is usually covered with an ointment bandage. Overall, a stay of about two hours should be expected.
How long does the healing process take?
Four to six weeks after surgery, the healing process is usually completed.
Can you feel the artificial lens in the eye?
Contrary to the contact lens, the artificial lens is not located on the sensitive cornea, but in the eye, so that it is not perceived as a foreign body.
Do you have to expect repulsive reactions?
Since the artificial lens consists of very well-tolerated plastics, rejection reactions are very rare.



 Independence of eyewear for seeing in the far and near, individually especially desired for occupation, in the household, in the leisure time, among other things.
Independence of eyewear for seeing in the far and near, individually especially desired for occupation, in the household, in the leisure time, among other things.